Cleaning Infected Blood
Biologists Develop Machine To Remove Viruses From Blood
Biologists Develop Machine To Remove Viruses From Blood
Editor- Nadim Dinani
Ref:- Discoveries and Breakthroughs in Science by Ivanhoe
Infectious disease experts designed a machine called the hemopurifier. It works much like a dialysis machine, using thin fibers to capture and remove viruses from the blood it filters. The machine requires the drawing of blood through an artery, which is sent through a tube into the machine, then back into the body. It can treat a number of illnesses.
 Every day, as many as 14,000 people are infected with HIV, the virus that leads to AIDs. There's no cure, but now a breakthrough -- a machine that could clean blood, keeping more and more people alive longer.
Every day, as many as 14,000 people are infected with HIV, the virus that leads to AIDs. There's no cure, but now a breakthrough -- a machine that could clean blood, keeping more and more people alive longer.John Paul Wobble, the inventor of this machine himself is an HIV patient.
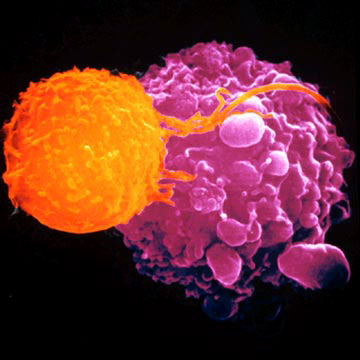
It is designed to mimic the natural immune response of clearing viruses and toxins before cells and organs can be infected. It is developed by infectious disease and biodefense experts. The hemopurifier works like a dialysis machine. Antibodies on these spaghetti-like fibers capture and remove viruses as blood filters through it.
 Your entire circulation flows through the cartridge about once every eight minutes. The entire process takes less than a few hours. It could help patients infected with HIV, hepatitis C, as well as people with the measles, mumps and the flu. The cartridge is able to selectively capture viruses.
Your entire circulation flows through the cartridge about once every eight minutes. The entire process takes less than a few hours. It could help patients infected with HIV, hepatitis C, as well as people with the measles, mumps and the flu. The cartridge is able to selectively capture viruses.A larger version of the machine would be used in a hospital, but a smaller one could be taken to emergencies. It could be a life-safer against the avian flu or bio-weapons like Ebola and small pox, giving people a chance to survive a deadly attack, whether it's from a terrorist or a virus.
The hemopurifier is also a leading treatment candidate to protect United States civilian and military populations from bioterror threats and emerging pandemic threats like the bird flu and dengue fever that are untreatable with drugs and vaccines.
REMOVING VIRUSES FROM BLOOD : The hemopurifier uses antibodies to remove viruses as blood filters through it. It is designed to filter out viruses and toxins before they attack organs. The method is very similar to dialysis, and can be used to help patients with HIV, Hepatitis C, the measles, mumps, the flu, and more. It can also begin working before doctors identify the cause of the illness.